The Electrocardiogram (ECG or EKG) is a vital diagnostic tool in cardiology, providing a graphical representation of the heart's electrical activity. Interpreting ECG strips is a crucial skill for healthcare professionals, enabling them to identify various cardiac conditions and abnormalities. This comprehensive guide aims to demystify the process of decoding ECG strips, offering a step-by-step approach to enhance understanding and accurate interpretation.
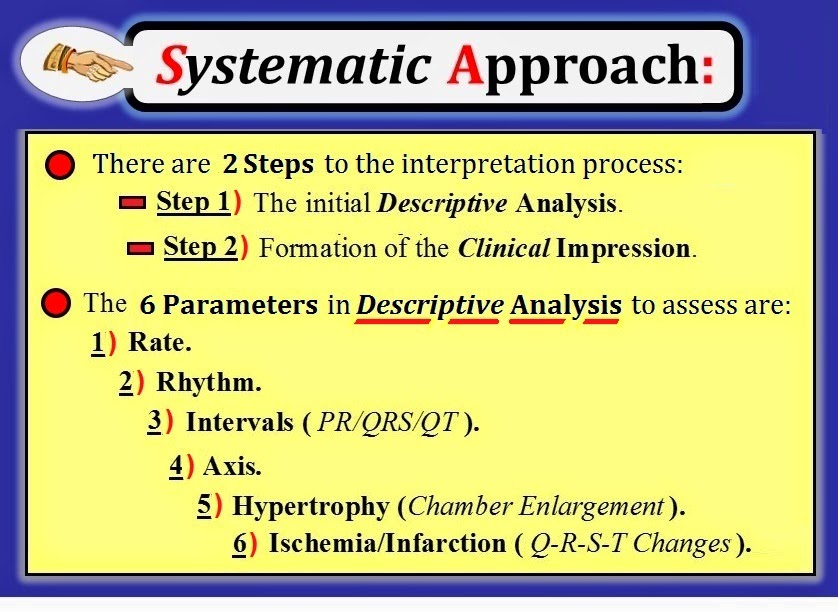
Step 1: Understand the Basics of ECG Interpretation
ECG interpretation is a systematic process that requires a solid foundation in understanding the basic principles. It involves recognizing the various waves, intervals, and segments that constitute an ECG strip. Each wave represents a specific phase of the cardiac cycle, providing insights into the heart’s electrical conduction and muscle activity.
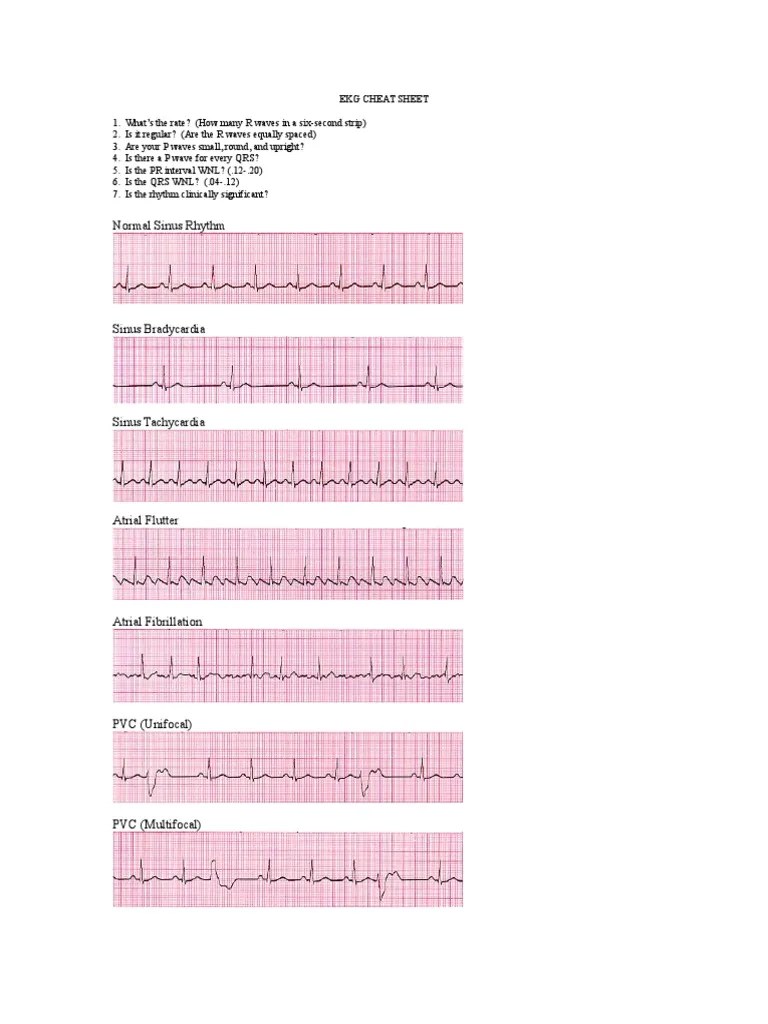
The primary waves of an ECG strip include the P wave, QRS complex, and T wave. The P wave signifies atrial depolarization, the QRS complex represents ventricular depolarization, and the T wave indicates ventricular repolarization. Additionally, there are important intervals such as the PR interval, QRS duration, and QT interval, which provide critical information about the heart's electrical conduction system.
Key Principles of ECG Interpretation
When interpreting an ECG, it is essential to consider the following principles:
- Rate: Evaluating the heart rate by counting the number of QRS complexes in a specified time frame, typically 6 seconds.
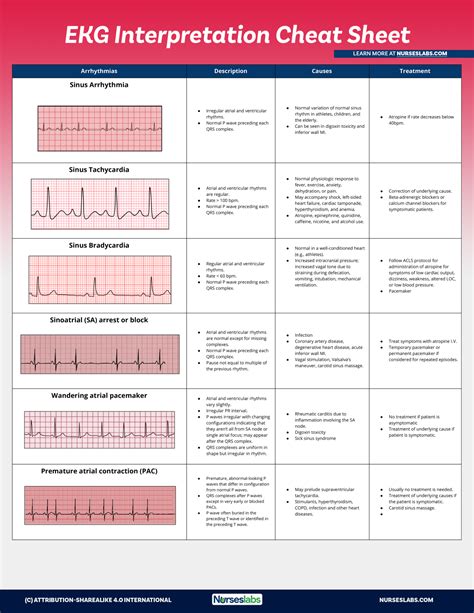
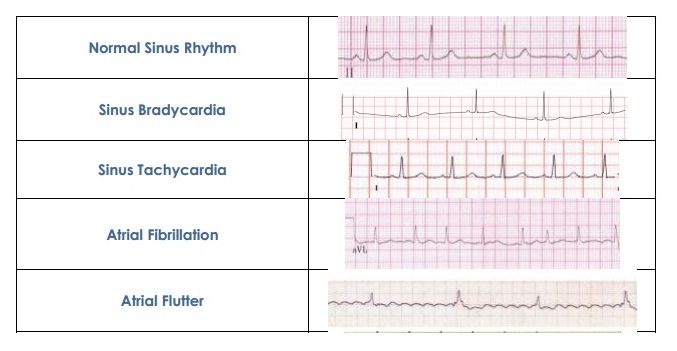
- Rhythm: Analyzing the regularity of the heart’s electrical activity, looking for any abnormalities in the timing and sequence of the waves.
- Axis: Determining the heart’s electrical axis, which provides information about the overall direction of the heart’s electrical activity.
- Intervals and Segments: Measuring the duration of intervals like the PR interval, QRS duration, and QT interval, as well as examining the ST segment for any elevation or depression.
Step 2: Assess the Quality of the ECG Strip
Before delving into the interpretation, it is crucial to assess the quality of the ECG strip. A well-recorded ECG strip should have clear, distinct waves and intervals without any significant artifacts or noise. Artifacts can distort the ECG and lead to misinterpretation, so it is essential to ensure the ECG is of good quality.
Factors to consider when assessing ECG quality include:
- Amplitude: The height of the waves should be consistent, with no significant variations or distortions.
- Noise: Minimal background noise or interference should be present, ensuring clear visualization of the waves.
- Baseline Wander: This refers to the fluctuating baseline of the ECG, which can be caused by breathing or movement. It should be minimal to avoid obscuring the waves.
- Lead Placement: Ensure that the leads are correctly placed on the patient's body, as improper placement can lead to inaccurate readings.
Step 3: Determine the Heart Rate and Rhythm
The first step in interpreting an ECG is to determine the heart rate and assess the rhythm. The heart rate is calculated by counting the number of QRS complexes in a specified time frame and multiplying by a factor. For example, if there are 15 QRS complexes in 6 seconds, the heart rate is calculated as (15 x 10) = 150 beats per minute.
Rhythm analysis involves evaluating the regularity of the heart's electrical activity. Regular rhythms have consistent intervals between successive QRS complexes, while irregular rhythms exhibit variations in timing. Common rhythm disturbances include atrial fibrillation, atrial flutter, and ventricular arrhythmias.
Calculating Heart Rate
To calculate the heart rate accurately, follow these steps:
- Identify the QRS complexes on the ECG strip.
- Count the number of QRS complexes in a specified time frame, typically 6 seconds.
- Multiply the count by a factor (usually 10) to obtain the heart rate in beats per minute.
Step 4: Evaluate the P Waves and PR Interval

The P wave represents atrial depolarization, and its characteristics provide valuable information about the heart’s electrical activity. P waves should be upright in lead II and should not exceed 2.5 mm in amplitude. Abnormal P waves can indicate atrial enlargement or atrial rhythm disturbances.
The PR interval measures the time it takes for the electrical impulse to travel from the sinus node to the ventricles. It should normally range from 0.12 to 0.20 seconds. Prolonged PR intervals can suggest conduction delays or first-degree heart block, while shortened PR intervals may indicate pre-excitation syndromes.
P Wave Abnormalities
Abnormal P waves can take various forms, including:
- Absent P waves: This may indicate atrial fibrillation or atrial flutter.
- Inverted P waves: Inverted P waves can be seen in certain conditions like left atrial enlargement or pericarditis.
- Prolonged P wave duration: Prolonged P waves may suggest atrial enlargement or conduction abnormalities.
Step 5: Analyze the QRS Complex and QRS Duration

The QRS complex represents ventricular depolarization, and its duration provides crucial information about the heart’s electrical conduction. The normal QRS duration should be less than 0.12 seconds. Prolonged QRS duration can indicate conduction abnormalities, such as bundle branch blocks or ventricular hypertrophy.
The QRS complex can also reveal the presence of certain cardiac conditions. For example, a wide QRS complex with a duration greater than 0.12 seconds may suggest ventricular arrhythmias or conduction disturbances.
QRS Complex Abnormalities
Abnormalities in the QRS complex can include:
- Wide QRS complex: As mentioned earlier, a wide QRS complex can indicate ventricular arrhythmias or conduction disturbances.
- Fragmented QRS complex: Fragmented QRS complexes are associated with myocardial scarring or infarction.
- Q waves: The presence of Q waves can suggest a previous myocardial infarction or ischemia.
Step 6: Assess the ST Segment and T Wave

The ST segment represents the period between ventricular depolarization and repolarization, while the T wave represents ventricular repolarization. The ST segment should be isoelectric, meaning it should be at the same level as the baseline. Deviations from the baseline, either upward or downward, can indicate cardiac ischemia or injury.
The T wave should be upright in most leads, with a normal amplitude. Inverted T waves can be seen in various conditions, including myocardial ischemia, left ventricular hypertrophy, or even physiological variations.
ST Segment and T Wave Abnormalities
Abnormalities in the ST segment and T wave can include:
- ST segment elevation: ST segment elevation can indicate acute myocardial infarction or pericarditis.
- ST segment depression: ST segment depression is often associated with myocardial ischemia or injury.
- T wave inversion: Inverted T waves can have various causes, including ischemia, left ventricular hypertrophy, or even physiological variations.
Step 7: Evaluate the QT Interval
The QT interval represents the time from the start of ventricular depolarization to the end of ventricular repolarization. It is measured from the beginning of the QRS complex to the end of the T wave. The QT interval should normally be less than 0.44 seconds in men and less than 0.46 seconds in women.
Prolonged QT intervals can be a marker of QT prolongation syndromes, which increase the risk of ventricular arrhythmias and sudden cardiac death. Shortened QT intervals may suggest certain genetic conditions or drug-induced QT shortening.
QT Interval Abnormalities
Abnormalities in the QT interval can include:
- Prolonged QT interval: As mentioned earlier, prolonged QT intervals can indicate QT prolongation syndromes or drug-induced QT prolongation.
- Shortened QT interval: Shortened QT intervals are less common but can be seen in certain genetic conditions or drug effects.
Step 8: Consider Lead Placement and Limb Lead Reversal

Accurate lead placement is crucial for obtaining reliable ECG readings. Inverted limb leads can lead to misinterpretation of the ECG, as it can cause a reversal of the P wave, QRS complex, and T wave.
It is important to ensure that the limb leads are correctly placed on the patient's body, with the right arm (RA) lead on the right arm, the left arm (LA) lead on the left arm, and the left leg (LL) lead on the left leg. The right leg (RL) lead is typically placed on the right hip or lower abdomen.
Limb Lead Reversal
Limb lead reversal occurs when the limb leads are placed incorrectly, leading to a reversal of the ECG waves. This can result in misinterpretation of the ECG, as the P wave, QRS complex, and T wave will appear inverted.
Step 9: Compare ECG Findings with Clinical Presentation
ECG interpretation should always be done in conjunction with the patient’s clinical presentation and medical history. Certain ECG findings may be nonspecific and can have multiple causes. Correlating the ECG findings with the patient’s symptoms, physical examination, and other diagnostic tests can help in making an accurate diagnosis.
For example, ST segment elevation on an ECG can indicate acute myocardial infarction, but it can also be seen in conditions like pericarditis or Prinzmetal's angina. Clinical correlation is essential to differentiate between these possibilities.
Step 10: Consult Reference Materials and Expert Opinions
Interpreting ECG strips can be complex, and it is always beneficial to consult reference materials and seek expert opinions. Textbooks, online resources, and consultation with experienced cardiologists or electrophysiologists can provide valuable insights and help in confirming or refining the ECG interpretation.
Reference materials should be up-to-date and evidence-based, ensuring that the information is accurate and reliable. Online resources, such as ECG interpretation guides and databases, can also be valuable tools for learning and refining ECG interpretation skills.
Frequently Asked Questions
What are some common ECG abnormalities to look for?
+Common ECG abnormalities include atrial fibrillation, atrial flutter, ventricular arrhythmias, bundle branch blocks, myocardial infarction, and QT prolongation syndromes. These conditions can be identified by evaluating the P waves, QRS complexes, ST segments, and QT intervals.
How can I improve my ECG interpretation skills?
+Improving ECG interpretation skills requires practice and exposure to a variety of ECG cases. Regularly reviewing ECG strips, consulting reference materials, and seeking guidance from experienced cardiologists or electrophysiologists can enhance your understanding and interpretation skills.
What are some common mistakes to avoid when interpreting ECG strips?
+Common mistakes to avoid include misinterpreting artifacts as true ECG waves, failing to consider the patient’s clinical presentation, and overlooking subtle ECG abnormalities. It is important to ensure the ECG strip is of good quality, correlate findings with clinical presentation, and consult reference materials or experts when in doubt.