Alzheimer's Disease is a progressive and irreversible neurodegenerative disorder that affects memory, thinking skills, and the ability to perform simple tasks. It is the most common cause of dementia, a term used to describe a decline in cognitive function that interferes with daily life. Alzheimer's Disease is a complex condition that poses significant challenges for both those diagnosed and their caregivers. Understanding the disease, its progression, and the available support systems is crucial for managing its impact on individuals and their families.
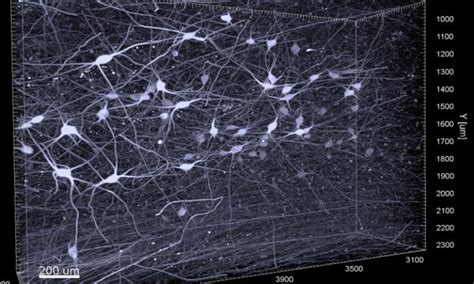
The Neurobiology of Alzheimer’s Disease

At its core, Alzheimer’s Disease is characterized by the abnormal buildup of proteins in the brain, leading to the formation of plaques and tangles. These plaques and tangles disrupt the communication between neurons, causing them to malfunction and eventually die. The loss of neurons and their connections leads to a decline in cognitive function and the characteristic symptoms of Alzheimer’s.
One of the key proteins involved in Alzheimer's is amyloid-beta. This protein is normally broken down and eliminated by the body, but in Alzheimer's, it accumulates and forms plaques. Another important protein is tau, which helps maintain the structure of neurons. In Alzheimer's, tau becomes abnormal and forms tangles, further disrupting neuronal function.
The Role of Neuroinflammation
Recent research has also highlighted the role of neuroinflammation in Alzheimer’s Disease. Neuroinflammation is the activation of the immune system in the brain, which can be triggered by various factors including the presence of amyloid plaques and tau tangles. This inflammatory response can further contribute to neuronal damage and cognitive decline.
Understanding the neurobiology of Alzheimer's is crucial for developing targeted treatments and interventions. While there is currently no cure for the disease, a deeper understanding of its underlying mechanisms has led to the development of potential therapeutic approaches, including medications that target amyloid plaques and tau tangles, as well as anti-inflammatory treatments.
Clinical Presentation and Progression

The clinical presentation of Alzheimer’s Disease varies widely among individuals, but certain hallmark symptoms are commonly observed. Early signs of the disease often include forgetfulness and difficulty with word-finding. As the disease progresses, individuals may experience more severe memory loss, particularly of recent events and newly learned information.
In addition to memory impairments, Alzheimer's can also affect other cognitive domains. Individuals may struggle with problem-solving, decision-making, and spatial awareness. They may have difficulty recognizing familiar faces or objects, and their language skills may deteriorate, leading to difficulties in communication.
Behavioral and Psychological Symptoms
Alzheimer’s Disease is not just a cognitive disorder; it can also have a significant impact on an individual’s behavior and psychological well-being. Some individuals may experience personality changes, becoming more irritable, anxious, or depressed. They may also exhibit aggressive or disruptive behaviors, such as wandering or becoming easily agitated.
Behavioral and psychological symptoms of Alzheimer's (BPSD) can be particularly challenging for caregivers to manage. These symptoms can arise at any stage of the disease and can significantly impact the quality of life for both the individual with Alzheimer's and their caregivers. It is important for caregivers to receive support and guidance in managing these symptoms effectively.
Diagnosis and Assessment
Diagnosing Alzheimer’s Disease involves a comprehensive evaluation by a healthcare professional, typically a neurologist or a geriatrician. The diagnostic process may include a detailed medical history, cognitive assessments, and brain imaging studies. While there is no single test for Alzheimer’s, a combination of these assessments can help confirm the diagnosis and rule out other potential causes of cognitive decline.
Cognitive assessments, such as the Mini-Mental State Examination (MMSE) and the Montreal Cognitive Assessment (MoCA), are commonly used to evaluate an individual's cognitive function. These assessments can help identify specific areas of cognitive impairment, such as memory, language, and executive function. Brain imaging studies, such as MRI and PET scans, can also provide valuable information about brain structure and function, helping to differentiate Alzheimer's from other forms of dementia.
The Importance of Early Diagnosis
Early diagnosis of Alzheimer’s Disease is crucial for several reasons. Firstly, it allows individuals and their families to access the appropriate support and resources to manage the disease effectively. Early diagnosis also provides an opportunity to initiate treatments that may slow down the progression of the disease and improve quality of life.
Additionally, early diagnosis can facilitate participation in clinical trials and research studies. Clinical trials are essential for developing new treatments and interventions for Alzheimer's. By participating in these trials, individuals with Alzheimer's can contribute to the advancement of medical knowledge and potentially benefit from innovative therapies.
Treatment and Management
Currently, there is no cure for Alzheimer’s Disease, but various treatment approaches aim to manage symptoms, slow down the progression of the disease, and improve the quality of life for individuals with Alzheimer’s and their caregivers.
Pharmacological treatments are commonly used to manage cognitive symptoms and behavioral disturbances. Cholinesterase inhibitors, such as donepezil and rivastigmine, are often prescribed to improve memory and cognitive function. These medications work by increasing the levels of acetylcholine, a neurotransmitter involved in memory and learning.
Non-Pharmacological Interventions
In addition to pharmacological treatments, non-pharmacological interventions play a crucial role in the management of Alzheimer’s Disease. These interventions focus on maintaining cognitive function, promoting independence, and improving overall well-being.
Cognitive stimulation therapy involves engaging in activities that challenge and stimulate the brain, such as puzzles, memory games, and social interactions. These activities can help slow down cognitive decline and improve quality of life. Music therapy and art therapy have also shown promise in improving mood, reducing agitation, and enhancing communication in individuals with Alzheimer's.
Physical exercise is another important aspect of non-pharmacological interventions. Regular physical activity has been shown to have cognitive benefits, including improved memory and attention. Exercise can also help manage behavioral symptoms, such as wandering and agitation, and improve overall physical health.
Caregiving and Support Systems

Caring for a loved one with Alzheimer’s Disease can be physically and emotionally demanding. Caregivers often face a range of challenges, including managing the individual’s cognitive and behavioral symptoms, providing assistance with daily activities, and coping with the emotional impact of the disease.
Support systems play a vital role in helping caregivers manage the demands of caregiving. These systems can include family members, friends, and professional caregivers. Support groups and community resources can provide emotional support, practical advice, and a sense of community for caregivers.
Respite Care and Self-Care
Respite care is an essential component of caregiving for individuals with Alzheimer’s. It involves temporary relief for caregivers, allowing them to take a break from their caregiving responsibilities. Respite care can be provided by family members, friends, or professional caregivers, and it can range from a few hours to several days.
Self-care is also crucial for caregivers to maintain their own well-being. Caregivers should prioritize their physical and mental health, including getting enough sleep, exercising regularly, and engaging in activities they enjoy. Taking time for self-care can help prevent caregiver burnout and improve overall caregiving quality.
Future Directions and Research
The field of Alzheimer’s research is constantly evolving, with new discoveries and advancements being made. Researchers are exploring various avenues to better understand the disease, develop effective treatments, and ultimately find a cure.
One area of focus is the development of biomarkers for early detection and diagnosis. Biomarkers are biological indicators that can be measured and used to assess the presence and progression of a disease. Identifying biomarkers for Alzheimer's could lead to earlier and more accurate diagnoses, allowing for earlier intervention and potentially slowing down the progression of the disease.
Emerging Therapies and Clinical Trials
Several emerging therapies are showing promise in the treatment of Alzheimer’s Disease. These include immunotherapies, which aim to target and remove amyloid plaques and tau tangles, and gene therapies, which focus on modifying the expression of genes involved in Alzheimer’s pathogenesis.
Clinical trials are ongoing to evaluate the safety and efficacy of these emerging therapies. Participation in clinical trials not only contributes to the advancement of medical knowledge but also provides individuals with Alzheimer's access to potentially innovative and effective treatments.
Conclusion

Alzheimer’s Disease presents significant challenges for individuals and their caregivers. However, with a better understanding of the disease, its progression, and the available support systems, it is possible to manage its impact and improve the quality of life for those affected. Ongoing research and the development of new treatments offer hope for the future, bringing us closer to a world where Alzheimer’s Disease is no longer a debilitating condition.
What are the early signs of Alzheimer’s Disease?
+Early signs of Alzheimer’s Disease often include forgetfulness, particularly of recent events and newly learned information. Individuals may also experience difficulty with word-finding, problem-solving, and decision-making. As the disease progresses, memory loss becomes more severe, and other cognitive domains, such as language and spatial awareness, may be affected.
How can caregivers manage behavioral symptoms in individuals with Alzheimer’s Disease?
+Managing behavioral symptoms in individuals with Alzheimer’s Disease requires a combination of strategies. These may include creating a calm and structured environment, establishing routines, and using distraction techniques. It is important for caregivers to remain patient and understanding, and to seek support from healthcare professionals and support groups.
What resources are available for caregivers of individuals with Alzheimer’s Disease?
+There are numerous resources available to support caregivers of individuals with Alzheimer’s Disease. These include support groups, both in-person and online, where caregivers can connect with others facing similar challenges. Caregiver training programs and educational resources can provide valuable information and strategies for managing caregiving responsibilities. Additionally, many communities offer respite care services, providing temporary relief for caregivers.