Gardnerella vaginalis, now known as Gardnerella or Bacteroides vaginalis, is a bacterium that plays a significant role in female reproductive health. This bacterium is a key player in the delicate balance of the vaginal microbiome, and its presence or absence can have notable effects on a woman's well-being. Understanding Gardnerella is crucial, especially for those experiencing vaginal health issues, as it can provide insights into potential causes and treatment options.
The Role of Gardnerella in the Vaginal Microbiome

The vaginal microbiome is a complex ecosystem teeming with various microorganisms, including bacteria, viruses, and fungi. Among these, Lactobacillus species typically dominate, creating an acidic environment that discourages the growth of harmful pathogens. However, Gardnerella is a unique bacterium that can exist in this environment without causing any issues, as long as it remains in balance with other microbial species.
In a healthy vaginal microbiome, Gardnerella exists in low numbers, often without causing any noticeable symptoms. However, when this balance is disrupted, Gardnerella can proliferate, leading to a condition known as bacterial vaginosis (BV). BV is characterized by a disruption in the normal vaginal flora, resulting in a decrease in beneficial Lactobacillus bacteria and an overgrowth of harmful bacteria like Gardnerella.
Symptoms and Diagnosis of Bacterial Vaginosis

The symptoms of BV can vary from person to person, but some common signs include:
- A thin, grayish-white vaginal discharge, often with a "fishy" odor.
- Itching or burning in the vaginal area.
- Discomfort during sexual intercourse.
- In some cases, no symptoms may be present, despite the presence of BV.
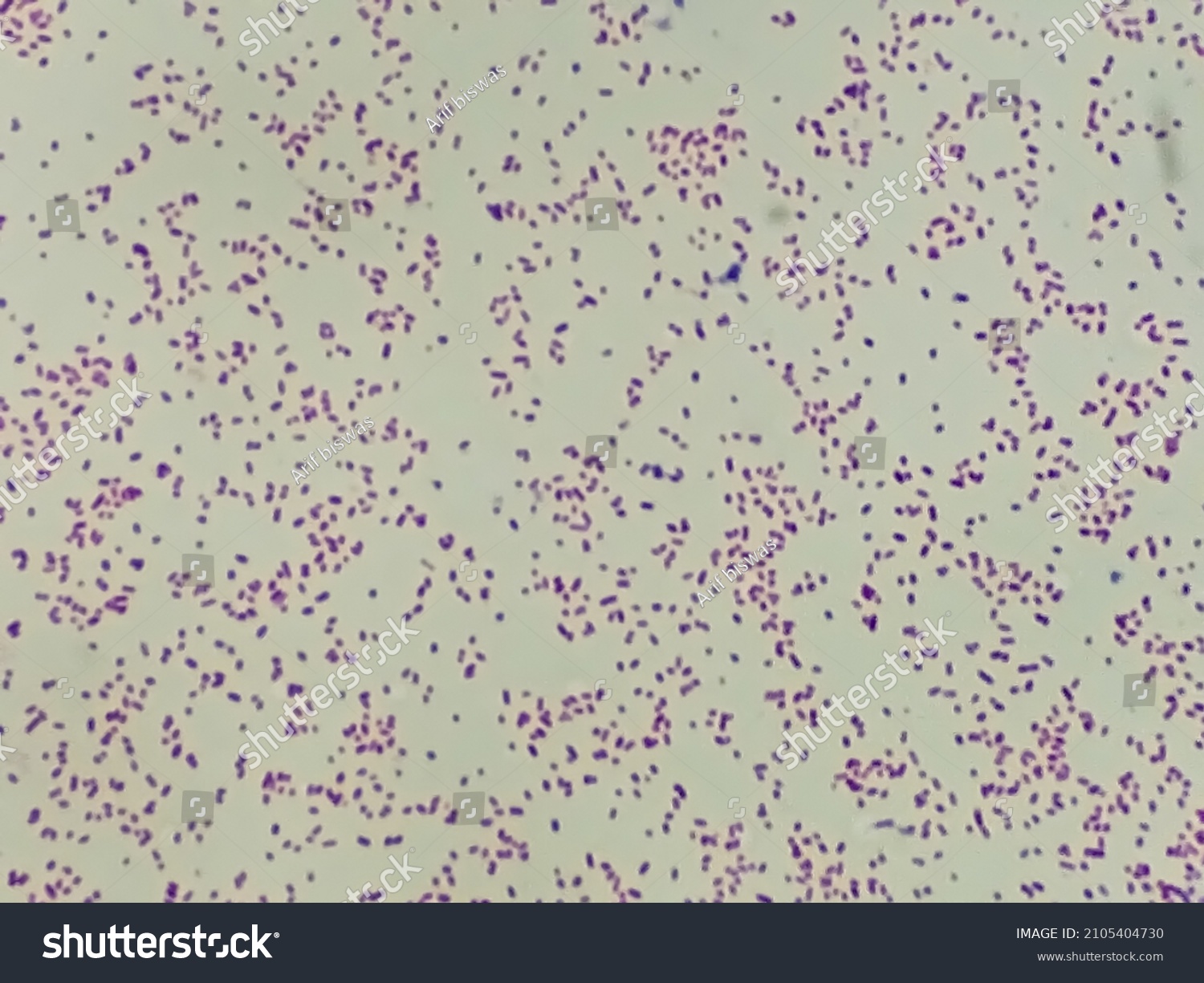
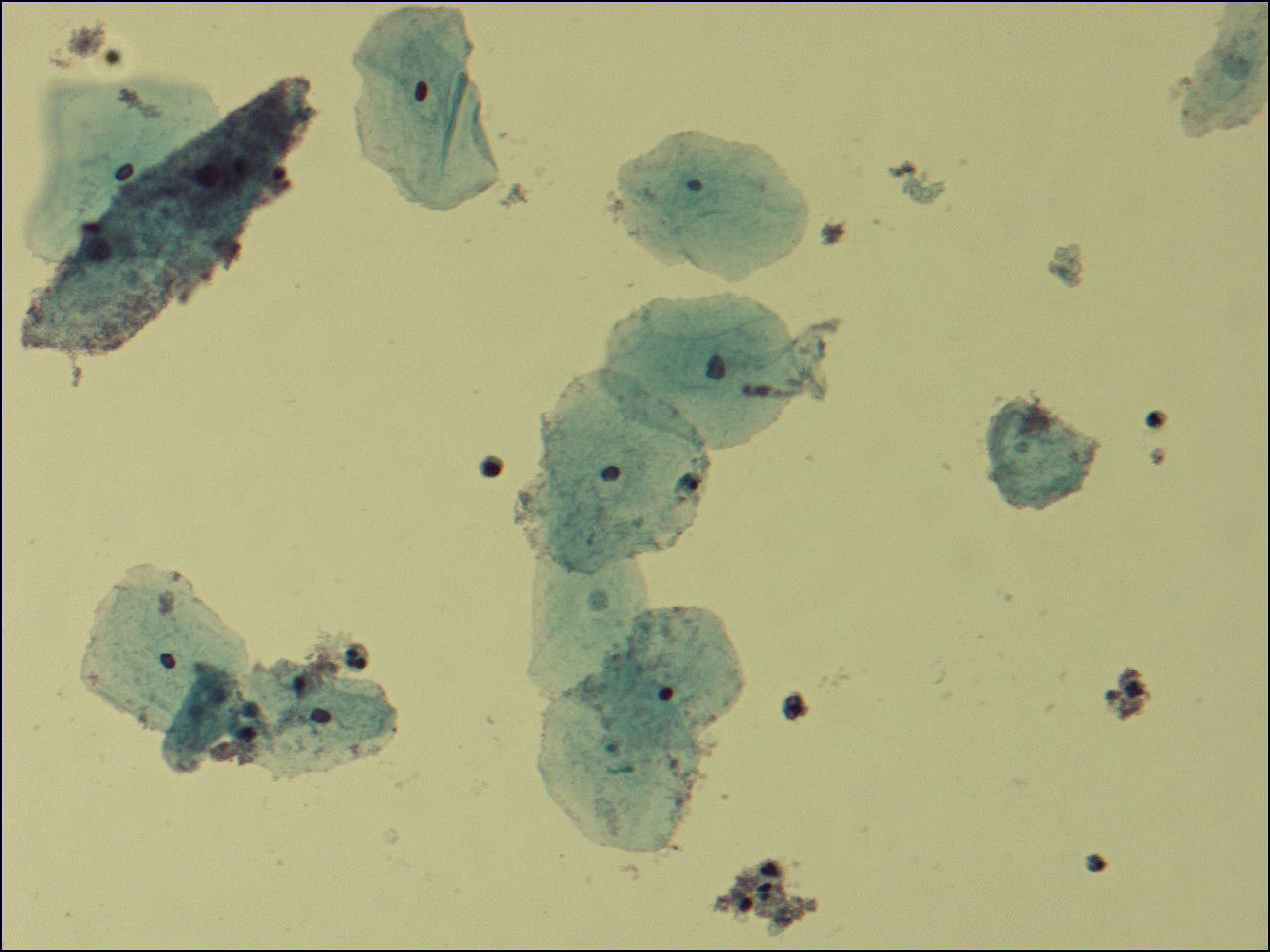
If you suspect you have BV, it's important to consult a healthcare professional. They can perform a vaginal examination and may take a sample of vaginal fluid for testing. This sample will be examined under a microscope to check for the presence of Gardnerella and other bacteria associated with BV.
Treatment and Management of Bacterial Vaginosis
The treatment for BV typically involves the use of antibiotics to restore the balance of the vaginal microbiome. Common antibiotics prescribed for BV include metronidazole and clindamycin. These medications can be taken orally or applied topically, depending on the severity of the infection and the individual's medical history.
In addition to antibiotics, maintaining good vaginal hygiene can help prevent BV. This includes avoiding douching, wearing breathable cotton underwear, and practicing safe sex. It's also important to avoid the use of harsh soaps or fragrances in the vaginal area, as these can disrupt the natural balance of the microbiome.
Prevention and Risk Factors

While BV can affect anyone with a vagina, certain factors can increase the risk of developing this condition. These include:
- Having multiple sexual partners or a new sexual partner.
- Engaging in unprotected sex.
- Using certain types of contraceptives, such as an intrauterine device (IUD) or spermicidal agents.
- Douching or using scented feminine hygiene products.
- Having a history of sexually transmitted infections (STIs) or other vaginal infections.
To reduce the risk of BV, it's important to practice safe sex, maintain good vaginal hygiene, and avoid douching or using harsh products in the vaginal area. Regular check-ups with a healthcare provider can also help identify and treat any potential issues early on.
Complications and Long-Term Effects
If left untreated, BV can lead to several complications. These include an increased risk of acquiring sexually transmitted infections (STIs), such as chlamydia or gonorrhea. BV can also increase the risk of pelvic inflammatory disease (PID) and may be a contributing factor in the development of cervical cancer.
In pregnant women, BV can increase the risk of preterm birth and low birth weight. It can also lead to complications during pregnancy, such as the development of urinary tract infections or postpartum endometritis.
Alternative Treatments and Natural Remedies

While antibiotics are the primary treatment for BV, some people may prefer to explore alternative or natural remedies. It's important to note that these remedies should not replace medical treatment, but they can be used as a complementary approach.
- Probiotics: Taking probiotic supplements or consuming probiotic-rich foods like yogurt can help restore the balance of good bacteria in the vagina.
- Garlic: Garlic has natural antimicrobial properties and can be inserted into the vagina as a suppository to help fight off harmful bacteria.
- Tea Tree Oil: Diluted tea tree oil can be applied topically to the vaginal area to help reduce bacterial overgrowth. However, it's important to dilute it properly to avoid irritation.
- Cranberry Juice: Cranberry juice is known for its ability to prevent urinary tract infections, and some believe it may also help with BV. However, more research is needed to confirm this.
The Future of Gardnerella Research

Research into Gardnerella and its role in vaginal health is ongoing. Scientists are working to better understand the complex interactions between different bacterial species in the vaginal microbiome and how these interactions can impact women's health. This research could lead to the development of more targeted and effective treatments for BV and other vaginal infections.
Additionally, there is growing interest in the use of probiotics and prebiotics to prevent and treat BV. Probiotics are live bacteria and yeasts that are beneficial for health, especially the digestive system. Prebiotics, on the other hand, are types of fiber that act as food for the good bacteria in the gut. By understanding how these substances can influence the vaginal microbiome, researchers hope to develop new strategies for maintaining vaginal health.
Conclusion

Gardnerella vaginalis, now known simply as Gardnerella, is a bacterium that plays a complex role in vaginal health. While it can exist in the vaginal microbiome without causing issues, an overgrowth of Gardnerella can lead to bacterial vaginosis. Understanding the symptoms, risk factors, and treatment options for BV is crucial for maintaining vaginal health and preventing potential complications. With ongoing research and a growing interest in natural remedies, the future of Gardnerella research looks promising, offering hope for more effective and holistic approaches to vaginal health.
What is the most common symptom of bacterial vaginosis (BV)?

+
The most common symptom of BV is a thin, grayish-white vaginal discharge with a strong, fishy odor.
Can BV be transmitted through sexual contact?

+
While BV is not considered a sexually transmitted infection (STI), having multiple sexual partners or engaging in unprotected sex can increase the risk of developing BV.
Are there any home remedies for BV?

+
While home remedies like probiotics, garlic, tea tree oil, and cranberry juice may help, it’s important to consult a healthcare professional for proper diagnosis and treatment. These remedies should not replace medical advice.
Can BV lead to more serious health issues if left untreated?

+
Yes, untreated BV can increase the risk of acquiring STIs, developing pelvic inflammatory disease (PID), and even contributing to the development of cervical cancer. It can also lead to complications during pregnancy.
How can I prevent BV?
+
Practicing good vaginal hygiene, avoiding douching, using scented feminine products, and engaging in safe sex practices can help reduce the risk of BV. Regular check-ups with a healthcare provider are also important for early detection and treatment.